An In-Depth Guide to the Male Reproductive System
Male Reproductive System
The human male reproductive system is the organ system responsible for producing male gametes (sperm cells) and delivering them for fertilization of the female ovum. It consists of a network of internal and external organs that work together to achieve sexual reproduction and also secrete hormones (like testosterone) that support reproductive function and the development of male secondary sexual characteristics. (As in all mammals, the male contributes sperm, while the female provides ova; the union of these gametes in reproduction perpetuates the species.) The primary components of the male system are the testes (male gonads), which generate sperm and hormones, and a series of ducts and glands that store, transport, and nourish the sperm, along with the penis which ensures delivery of sperm into the female reproductive tract.
The major functions of the male reproductive system include producing, maintaining, and transporting sperm (the male reproductive cells) along with the seminal fluid, discharging sperm within the female reproductive tract during intercourse, and secreting male sex hormones such as testosteronemy.clevelandclinic.org. These functions enable sexual reproduction and also contribute to urinary excretion (via shared structures).
Educational resources often present this topic through labeled diagrams of the male reproductive system and organized notes. Accordingly, the following sections provide a detailed yet concise set of male reproductive system notes (suitable for a PDF handout), covering the structure of the male reproductive system, key organs with their anatomy and functions, and the physiological processes involved.
{getToc} $title={Table of Contents} $count={Boolean} $expanded={Boolean}
Structure of the Male Reproductive System
The male reproductive system (male genital system) is composed of primary sex organs and secondary (accessory) reproductive organs. The primary organs are the testes (singular: testis), which are the male gonads that produce sperm and hormones. The secondary structures include a series of ducts (the epididymides, vas deferens, ejaculatory ducts, and urethra) that transport sperm, accessory glands (the seminal vesicles, prostate gland, and bulbourethral glands) that secrete fluids to form semen, and the external genitalia (the penis and scrotum)britannica.com. In humans, the external organs (penis and scrotum, which contains the testes) lie outside the abdominal cavitymy.clevelandclinic.org, while the remaining components are located internally within the pelvis.
Testes (Testicles)
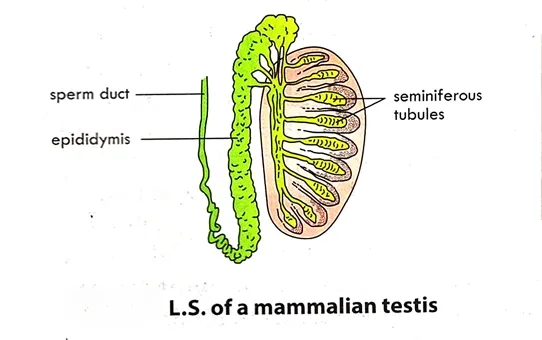
The testes are the primary male reproductive organs (gonads), located inside the scrotum. Each testis is an oval-shaped gland ~4–5 cm in length, enclosed by a tough fibrous capsule, and suspended outside the abdominal cavity in the scrotal sac. The testes produce sperm cells and also secrete the male sex hormone testosterone, which is crucial for male reproductive function and the development of male secondary sexual characteristics (facial hair, deeper voice, etc.).
Internally, each testis contains hundreds of tightly coiled seminiferous tubules where sperm production (spermatogenesis) takes place. These fine tubules are packed into wedge-shaped lobules and lined with germ cells that continuously proliferate and differentiate into mature spermatozoa. Embedded between the tubules are endocrine cells called Leydig cells, which release testosterone into the bloodstream. Remarkably, the testes produce on the order of 200–300 million sperm cells per day in an adult male, although roughly only half (about 100 million) of these ultimately become viable spermen.wikipedia.org. To facilitate sperm production, the testes are situated in the cooler environment of the scrotum (a few degrees below core body temperature, ~34–35 °C); this lower temperature is essential for optimal spermatogenesis.
Epididymis
The epididymis is a long, coiled tubular organ that lies along the posterior (back) side of each testis. It serves as a storage and maturation site for sperm. Sperm produced in the testis are initially immature and incapable of fertilization; they move into the epididymis, where they are stored and undergo final maturation.
An epididymis can reach about 6 meters in length when uncoiled, though it is compacted into a comma-shaped structure (~4 cm) atop each testis. Over a period of ~2–3 weeks, sperm travel slowly through the coils of the epididymis and gain motility and the capacity to fertilize an eggmy.clevelandclinic.org. During sexual arousal and just prior to ejaculation, smooth muscle in the epididymis wall contracts, propelling the mature sperm into the next duct, the vas deferensmy.clevelandclinic.org.
Vas Deferens (Ductus Deferens)
The vas deferens is a thick-walled, muscular tube that transports sperm from the epididymis toward the urethra during ejaculation. Each testis has its own vas deferens: it begins at the tail end of the epididymis and ascends through the spermatic cord (a structure containing the vas, blood vessels, nerves, and lymphatics) into the pelvic cavity.
Each vas deferens is about 30–45 cm long. It travels upward from the scrotum, passes through the inguinal canal into the pelvis, then courses posterior to the bladder. Within the prostate region, the vas deferens from each side joins with the duct of the corresponding seminal vesicle to form a short ejaculatory duct. These ejaculatory ducts then connect to the urethra inside the prostate gland. The function of the vas deferens is to conduct mature sperm from the epididymis to the ejaculatory duct (and ultimately into the urethra) by peristaltic contractions of its smooth muscle wallmy.clevelandclinic.org.
Seminal Vesicles
The seminal vesicles are a pair of accessory glands located behind the bladder and above the prostate gland. Each seminal vesicle is a sac-like gland (~5 cm long) that opens into the corresponding ejaculatory duct. The seminal vesicles produce a thick, yellowish secretion that constitutes the majority of the seminal fluid.
Seminal vesicle fluid is rich in fructose (a sugar that provides an energy source for sperm) and other substances that promote sperm motility and viability. In fact, the seminal vesicles contribute about 60–80% of the volume of semenmy.clevelandclinic.org. This secretion is alkaline, which helps neutralize the acidic environment of the female reproductive tract, and it contains prostaglandins that may assist in stimulating contractions in the female tract to aid sperm movement. The fructose in the semen is crucial because sperm cells rely on it for the energy needed to swim.
Prostate Gland
The prostate gland is a single, walnut-sized gland situated just below the urinary bladder and encircling the upper part of the urethra (the prostatic urethra). The prostate is an exocrine gland of the male reproductive system and it adds a milky fluid to the semen. It is firm in texture and is composed of glandular tissue and smooth muscle, enclosed in a fibromuscular capsule.
The prostate’s secretion makes up roughly 20–30% of semen and is a thin, milky, slightly alkaline fluiden.wikipedia.org. This prostatic fluid contains enzymes (such as prostate-specific antigen, PSA) and zinc, and its alkalinity helps neutralize the acidity of the vaginal tract, thereby protecting sperm and improving their motility once inside the femaleen.wikipedia.org. During ejaculation, smooth muscle in the prostate contracts to expel prostatic fluid into the urethra, where it mixes with sperm and seminal vesicle fluid. (Notably, the prostate gland is present in all male mammals, though its size, anatomy, and specific composition of secretions vary among speciesen.wikipedia.org.)
Bulbourethral Glands (Cowper’s Glands)
The bulbourethral glands are two small, pea-sized glands located on either side of the urethra, just below the prostate gland (within the urogenital diaphragm of the pelvic floor). They are considered accessory glands of the male reproductive system.
The primary product of the bulbourethral glands is a clear, slippery secretion released just before ejaculation (often called pre-ejaculate). This fluid is alkaline and serves to lubricate the urethra and neutralize any residual acidity from urine in the urethral passagemy.clevelandclinic.org. By clearing and buffering the urethra, the bulbourethral secretion helps protect sperm as they pass through the urethra during ejaculation. The volume of this pre-ejaculatory fluid is small (a few drops) but it plays an important role in making the urethral environment more hospitable for sperm.
Urethra
The urethra in males is a dual-purpose tubular structure that is part of both the urinary and reproductive systems. It runs from the bladder, through the prostate gland, and along the length of the penis, opening at the tip of the glans penis. In the context of reproduction, the urethra serves as the final duct through which semen is ejaculated out of the body. (It also carries urine from the bladder during urination, but never at the same time as semen discharge—reflex mechanisms prevent the simultaneous flow of urine and semen.)
Anatomically, the male urethra is subdivided into three sections: the prostatic urethra (segment passing through the prostate), the membranous urethra (short segment passing through the urogenital diaphragm of the pelvic floor), and the spongy (penile) urethra (long segment running through the penis). During ejaculation, semen from the ejaculatory ducts is deposited into the prostatic urethra and then propelled through the penile urethra to the outside. The urethral lining also contains mucus-secreting glands that assist in lubrication. At the moment of orgasm, a sphincter muscle at the bladder neck closes to prevent urine release, ensuring that only semen travels through the urethra.
Penis
The penis is the external copulatory organ of the male, specialized to deposit sperm into the female reproductive tract. It is a cylindrical, elongated organ suspended outside the body, and it contains the urethra as well as erectile tissues. Structurally, the penis is composed of three columns of erectile tissue: two dorsal corpora cavernosa and one ventral corpus spongiosum (which surrounds the urethra). The distal end of the corpus spongiosum forms the glans penis, which is the sensitive, expanded tip. The penis is covered by skin; in uncircumcised males, the glans is covered by a retractable fold of skin called the foreskin (prepuce).
When sexual stimulation occurs, blood fills the spaces in the erectile tissues, causing the penis to become engorged and rigid (an erection). This erect state enables penetration of the female vagina during intercourse. The primary function of the penis is to serve as the copulatory organ, delivering semen into the female genital tract during ejaculation. Additionally, the penis provides a means for urination, as it contains the terminal portion of the urethra. The design of the penis—with its erectile mechanism—ensures that sperm can be effectively deposited deep in the vagina, increasing the likelihood of successful fertilization of the ovum.
Scrotum
The scrotum is the pouch of skin, connective tissue, and muscle that hangs below the base of the penis and houses the testes. Externally, it appears as a single sac, but internally it is divided into two compartments (one for each testis) by a septum. The scrotal wall contains the dartos muscle (a layer of smooth muscle in the skin) and it is connected to the cremaster muscles (extensions of the internal oblique muscles) that descend into the spermatic cords.
The scrotum’s primary role is thermoregulation of the testes. Sperm production requires a temperature about 2–3 °C lower than normal core body temperature. The scrotal musculature can reflexively adjust the position of the testes: in cooler conditions, the dartos and cremaster muscles contract to pull the testes closer to the warmth of the body, and in warmer conditions, they relax to let the testes hang farther from the body heat. This helps maintain an optimal testicular temperature (~34 °C) for healthy sperm developmentsbivf.com. The scrotum also protects the testes from mechanical injury to some extent, and it contains blood vessels and nerves that support testicular function.
Sperm Production and Pathway of Ejaculation
Spermatogenesis
Spermatogenesis is the process of production of sperm cells (spermatozoa) by the division of spermatogenic cells in the germinal epithelium. Sperm production are controlled by follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary gland and by testosterone from the testes.
The outermost cells of a seminiferous tubule are known as spermatozoid or primordial germinal cells. They are formed from the germinal epithelium. These cells divide to form diploid spermatogonium (plural: spermatogonia). The spermatogonium divides by mitosis and undergoes changes to become a primary spermatocyte.
Each primary spermatocyte, divides in the first meiotic division to form two haploid secondary spermatocytes.
In the second meiotic division, each secondary spermatocyte divides to form two haploid spermatids. Each spermatid attaches to a supporting cell (Sertoli cell) and develops a flagellum to form a sperm cell.
Sperm cells are carried into the epididymis where they are temporally stored and mature.
A mature sperm cell consists of a head, middle piece, and flagellum or tail. The flattened head is composed of a compact nucleus containing 23 chromosomes. The anterior portion of the head is covered by a cuplike structure, called the acrosome. The acrosome contains an enzyme that helps the sperm cell penetrate the female sex cell. The body contains mitochondria, where ATP is formed, required for lashing the flagellum.
Structure of the Sperm
During sexual climax (ejaculation), a series of muscular contractions expels the sperm along with glandular secretions, forming semen. The sequence of events is as follows:
- Sperm are produced in the testes (within seminiferous tubules) and then move into the epididymis as immotile, immature cells.
- In the epididymis, the sperm mature and are stored until ejaculation.
- Upon sexual arousal, the mature sperm are propelled from the epididymis into the vas deferens by contraction of smooth muscles.
- The sperm travel through the vas deferens into the pelvic cavity. As each vas deferens approaches the prostate, it joins with a duct from a seminal vesicle to form an ejaculatory duct; the seminal vesicles secrete a fructose-rich fluid that mixes with the sperm.
- The two ejaculatory ducts (one from each side) empty into the prostatic urethra. Here, the prostate gland adds its milky, alkaline secretion to the mixture, further contributing to what is now semen.
- Just prior to ejaculation, the bulbourethral glands release a few drops of clear fluid into the urethra. This pre-ejaculate fluid lubricates the urethral lining and neutralizes any acidic residue, preparing the way for the semen.
- Finally, semen (containing sperm plus the combined fluids from the seminal vesicles, prostate, and bulbourethral glands) is forcefully expelled through the urethra and out of the penis during ejaculation. This expulsion is aided by rhythmic contractions of pelvic floor muscles and the muscles surrounding the urethra.
In a typical human ejaculate, the semen volume is about 2–5 mL, containing hundreds of millions of sperm cells suspended in glandular fluids. Once deposited in the female reproductive tract, the sperm begin their journey to seek out and fertilize an egg (ovum). The entire male reproductive process – from spermatogenesis in the testes to ejaculation via the penis – is a highly coordinated physiological sequence that ensures sperm are produced, nourished, and delivered to the site of fertilization.
Diagrams and Visual Representations
Figure: Simplified cross-sectional diagram of the male reproductive organs (side view), showing the internal anatomy including the bladder (above the prostate), the prostate gland (encircling the urethra), the seminal vesicles (behind the bladder), and the path of the duct system out through the penis. Such male reproductive system diagrams are valuable for understanding the spatial relationships among structures. In a real male reproductive system, as seen in medical imaging or dissection, the organs appear in three-dimensional detail, but labeled schematics like this help simplify and identify each component. Both anterior (front) and lateral (side) view diagrams are commonly used in textbooks and notes to illustrate the male genital anatomy from different perspectives (the side view, as shown, highlights how the internal glands connect to the urethra).
Visual aids often accompany academic notes on the male reproductive system – for instance, many students refer to textbook figures or male reproductive system diagram (PDF) resources for study. These diagrams typically label all major parts (testes, epididymis, vas deferens, seminal vesicles, prostate, urethra, penis, etc.) and sometimes use color-coding to distinguish between different types of structures (e.g., glands vs. ducts). By comparing diagrams to actual anatomical models or images, one can gain a comprehensive understanding of how the male reproductive organs are positioned and how they function together during the process of reproduction.
Summary Table of Organs and Functions
The table below summarizes the main organs of the male reproductive system, their basic structure/location, and their primary functions:
| Organ/Part | Structure & Location | Primary Function(s) |
|---|---|---|
| Testes (Testicles) | Pair of oval gonads located in the scrotum; contain coiled seminiferous tubules | Produce sperm (spermatogenesis) and secrete male sex hormones (primarily testosterone) |
| Epididymis | Long coiled tube attached to posterior of each testis (within scrotum) | Stores sperm and allows them to mature (gain motility and fertilizing capacity) |
| Vas Deferens | Thick muscular duct extending from epididymis, through spermatic cord into pelvic cavity | Transports mature sperm from scrotum toward urethra (during ejaculation) |
| Seminal Vesicles | Two glandular sacs located behind bladder; ducts join vas deferens | Secrete fructose-rich, alkaline fluid (~60–80% of semen) that nourishes sperm and enhances motility |
| Prostate Gland | Single walnut-sized gland below bladder; surrounds the urethra at base of bladder | Produces milky, slightly alkaline fluid (~20–30% of semen) that helps neutralize vaginal acidity and supports sperm viability |
| Bulbourethral Glands | Two small (pea-sized) glands beneath the prostate, beside the urethra in the pelvic floor | Release a clear lubricating fluid (pre-ejaculate) that neutralizes residual urine acidity in urethra and lubricates the passage |
| Urethra | Single tube running from bladder through prostate and penis (prostatic, membranous, penile sections) | Conveys semen out of the body during ejaculation (and urine during urination, at separate times) |
| Penis | External cylindrical organ composed of erectile tissue; contains the distal urethra | Copulatory organ that delivers semen into the female tract; also serves as the organ of urination |
| Scrotum | Pouch of skin and muscle divided into two compartments, hanging below the pelvic region | Houses and protects the testes; regulates testicular temperature (by moving testes closer to or away from body) |
Conclusion
The male reproductive system is essential for reproduction, sexual function, and overall health. Understanding its anatomy and functions is crucial for maintaining reproductive health and addressing potential issues.
Get Your Free PDF!
Download our comprehensive guide to
Male Reproductive System to boost your knowledge.
Download PDF
Click the button above to get instant access to the PDF.
Get Your Free PDF!
Download our comprehensive guide to
Male Reproductive System to boost your knowledge.
Download PDFClick the button above to get instant access to the PDF.
Further Resources
Related Post on Biology Topics
Click Here for WAEC Past Questions and Answers on Reproduction in Human




.webp)